
The first thing to understand is that no matter what anyone tells you, this is not your fault. There is nothing that you did or did not do that caused your baby to have a cleft palate. There are very rare exceptions for this rule like the mother may have had a significant vitamin deficiency or may have been taking an anti-seizure medication before she knew she was pregnant. There is also the chance that either parent may be a carrier of a gene that might increase the risk of a child with a cleft but again that is not your fault. We do know that a cleft palate occurs in one out of every 1000 children born in the US.
We do not consider cleft palate a birth deformity, because all of us (You, me, Brad Pitt and even Angelina Jolie), while in the womb, had a cleft as part of our embryologic development. Immediately after conception, the fetus starts as one cell. As the cells double in number, the head is made of 3 separate growths of tissue, the largest from the back that includes the head, brain, forehead, nose, center of the upper lip, and the front 4 teeth. A separate outgrowth from each side contains the ear, eye, cheek, upper jaw to the canine tooth, and the lower jaw to the midline. At approximately the fifth week of development, these three tissue blocks fuse together and fusion lines can be seen as the philtral column on our normal lips. Occasionally, amongst the billions of steps in fetal development, these tissue planes do not fuse all the way creating a unilateral or bilateral cleft.
We believe that children born with a cleft palate are just like everybody else but the normal process of development did not quite finish, and that it is our team’s opportunity and responsibility to finish this process. We have been taking care of children who now have children of their own and live very normal lives having graduated from high school and attended college.
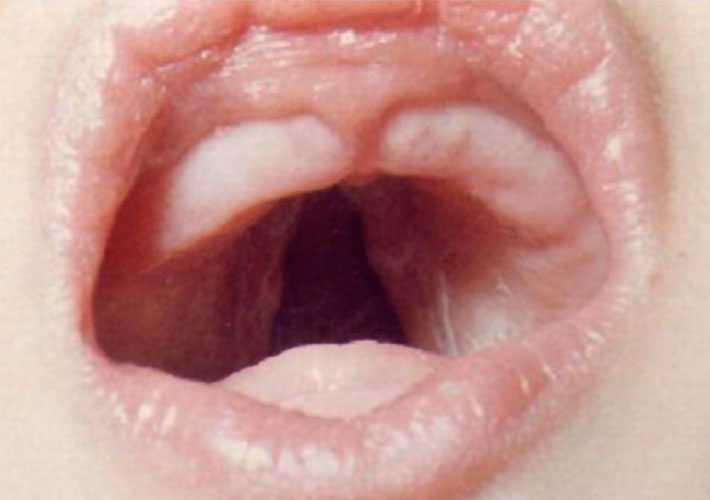
You have probably noticed that there are many different types of cleft palate. Classification of a cleft palate is a little bit different than we usually described how much of the palate is involved. Instead of saying a complete or incomplete cleft palate, we generally describe which tissues of the palate are involved. The anatomy of the palate involves the uvula, soft palate including the muscles of the soft palate which elevated the palate for speech, and then the hard portion of the palate (roof) to just behind the gums, and the alveolar or gums segment. One additional term that we use to designate the severity of the cleft might be to describe it as being wide or extremely wide in the gap between the 2 sides of the cleft.
As a metaphor, I would like to use a parka with two zippers; when the top zipper is zipped to the top, your parka is effectively closed. There is a bottom zipper that allows you to partially open the jacket from the bottom. Then, if you think about it, there are an infinite number of variations of the position of the two zippers from completely closed to completely open. Think of the cleft palate like your parka with 1 zipper at the back of the uvula and the other zipper at the tip of the gums. If we open just the back half of the palate we would have a cleft palate involving the soft palate only. Just like your parka with the two zippers, there is an infinite number of possibilities from completely closed to completely open. Because of the great variety and types of clefts, this makes it difficult to relate to the information you receive from a Google search. You do not know the severity of the cleft or the quality of care that that patient may have received.


Frequently Asked Questions
Love your baby like there is no tomorrow and thank the powers that be that you have been blessed with such a beautiful perfect little life. When you get around to it, please call our team coordinator at 208-433-1736 and send us a few photos of your new amazing baby so that we can get an idea of the type of cleft and what structures are involved. We will then come directly to your room or contact you by phone that day and make sure that everything is set up. If you are in a hospital setting, we will also talk to the nurses and doctors taking care of your baby.
If your baby has a cleft lip only, and the palate is intact from the gums back to the uvula, then very little needs to be done. Your baby can breast-feed if you would like or you can bottle feed from any bottle of your choice. Take lots and lots of photographs and we will arrange to repair your baby’s cleft lip at approximately 8 weeks of age. You will bond with this new baby and his or her cleft and although you will anticipate the date that we repair it, you will always miss the appearance of that sweet little smile.
If your baby was born with a cleft lip and palate, then we will need to train you with a special cleft palate bottle. The cleft palate bottles we most commonly use are the Dr. Brown cleft palate nurser, the Habermann, and the Pigeon bottle. Each of them has their own advantages and disadvantages and we will recommend the one that works best based on the shape of your baby’s mouth.
If your baby has a cleft palate then we do not recommend breast-feeding. We believe that the best source of nutrition for your newborn baby is his or her mother’s breast milk but we have a structural problem with a cleft palate that makes breast-feeding difficult. The first, is that children with a cleft palate are unable to generate a suction making it difficult for them to get the milk out of the breast. The second problem is that it is easy for them to get too much milk and have a slightly higher risk of getting some of that milk into the lungs. This occurs during the milk let down reflex when the breasts can actually spray shortly after initiating breast-feeding. This extra volume from the milk let down reflex can be difficult for your baby to manage. Because of these problems, we recommend pumping breast milk if you are able and then feeding your child with one of the cleft palate bottles that we have recommended.
The special cleft palate bottles do not rely upon suction to get the milk out. They can be best thought of as bite bottles. There is a small one-way diaphragm between the nipple and the bottle contents that only allows milk to fill the nipple. When your baby bites down on the nipple, the milk is expressed through the opening of the nipple so that he or she can then swallow it. The different cleft palate nipples all have a different shape, and a different method for controlling the amount of milk flow through the nipple (less for newborns and more for older infants), and usually one is best suited for your child’s mouth shape.
An infant with a cleft palate (whether they have a cleft lip or not), is best fed using one of the recommended cleft palate bottles. Feeding is difficult because of 2 main issues: Getting enough volume, and handling and excess of volume. It is easy to understand that with your baby’s inability to create a suction that they need to bite the nipple of a special cleft palate bottle to be able to express the contents into their mouth so they can swallow it. The nipple needs to be held in a way so that they can compress it between her tongue and a part of their palate that is intact. This takes quite a bit of practice for both you the parent and for your infant. This is a little bit more challenging with a wide unilateral or bilateral cleft lip because the nipple always wants to slide up into the nose. Just keep trying, you will get the hang of it. To assist you, we will have one of our cleft lip and palate team’s feeding specialists come to your bedside and help you and your baby learn how to use the new bottle.
The second challenge in feeding your baby with a cleft palate is that they can struggle with getting too much volume. To explain this point, I would like to use an example. Imagine you are in the passenger seat of a car and you just opened a 20 ounce bottle of your favorite soda beverage. As you begin to drink, the driver of the car suddenly accelerates with the green light allowing some of the soda you are drinking to unexpectedly and surprisingly hit the back of your throat causing you to cough and sputter. When we drink, we take the fluid into the front of our mouth and then our brain carefully coordinates sending the fluid past our tongue, over the closed epiglottis, and into our esophagus. This is a highly coordinated multistage process that we do not even think about. Your cough reflex is initiated if fluid gets into the back of the throat when you do not expect it.
When you feed your baby with a cleft palate, it is very easy for excess milk to get into the back of their throat which will most certainly make them anxious and may make them feed poorly. To control the volume your baby gets and to make sure that it does not get into the back of their throat unexpectedly, we recommend that your child be fed in the near upright position rather than laying flat in your arms the way we normally feed other babies. If extra milk accumulates in your infant’s mouth, and they are in the near upright position, then the extra milk will come out the corners of their mouth rather than gurgle in the back of their throat potentially tickling their vocal cords.
It is also important that when you feed your baby, carefully listen to them. I mean really listen. You will hear 3 types of sounds, biting on the bottle, swallowing, and breathing. You will notice that your baby will bite several times on the bottle, swallow, and then take several breaths. Sometimes it helps to pull the nipple out a little bit while your baby is taking these breaths. If your baby is making sounds as if struggling from too much fluid in the back of their throat, you need to move them into the face down position as quickly as possible so any extra fluid can easily drain out their mouth. Very simply and quickly, drop the bottle, place your hand on your baby’s face and move them face down and the extra milk will drain out of their mouth and into your palm (You do not need to pat them on their back). In a few short seconds, they usually clear their airway and then can be sat upright again to continue to feed.
Your doctors and nurses will carefully look at your baby to make sure that everything else is ok. All new infants are examined in this manner including listening to their breath sounds, listening to their heart, looking carefully at extremities, checking reflexes, as well as listening to and feeling the abdomen. Most hospitals require that your child receive a hearing exam. Chances are, if your baby has a cleft palate, the child will not pass this newborn hearing screen (do not be alarmed, this is normal). Most patients born with a cleft palate have fluid in their ears behind the eardrums. The audiologist we will arrange for a follow-up test in a few weeks. (see section on hearing issues) Sometimes, additional tests might be needed depending upon the exam findings like a cardiac echo or a renal ultrasound.
Most of our patients are big healthy children and we just need to focus on growing and weight gain. Occasionally, we have a child who does not feed well or gain weight appropriately and we have them meet with our feeding specialists. Occasionally, we have a child that just cannot meet the feeding volumes and we might need the help of a temporary feeding tube. This tube goes through the nostril and down into the baby’s tummy. The tube is used for any remaining milk after feeding for 15-20 minutes (Whatever is left over in the bottle is placed down the tube). We can give specific instructions on how to do this if necessary. Normally, the tube is used less and less over the next few weeks and eventually is removed.
Another thing to carefully watch for his breathing issues. Occasionally, we can have a child who is silently aspirating. This means, as they are feeding, a small amount might be getting past the vocal cords and might be entering the lungs. If a child appears to be having some breathing issues, our team which includes the help of the primary care physician, can examine your child to determine if a swallow study is warranted. A swallow study involves feeding the baby with the nipple with a small amount of barium added to the milk and then an x-ray movie is taken both from the front and the side. The fluid can be seen on x-ray and if any entered the lungs it would be quite evident. Although rare, we do occasionally identify a child who is silently aspirating. We would then take them off the bottle and put them on feeds through the nasogastric tube only. Usually, after a month, we recheck a swallow study to see if they have improved. Most children do, but occasionally if the child continues to have silent aspiration, it may be recommended that they be seen by a gastroenterologist and have a gastrostomy tube placed.
If a child with a cleft palate is having breathing issues and is not aspirating based on swallow study, they might need to have the back of the throat examined by an ear nose and throat specialist utilizing a special fiberoptic scope to see if there might be any anatomic issues. This is usually a very easy study that can be performed in the clinic setting by our cleft team otolaryngologist.
Most children with cleft palate will only require one cleft palate repair (palatoplasty) as described in the previous section. We need to look your child over very carefully especially if she or he has a cleft palate only, because children with cleft palate only can have a higher incidence of other issues like breathing problems or association with other syndromes like sticklers Syndrome and Pierre Robin Sequence.
Pierre Robin sequence involves children who have a very wide U-shape cleft palate, extremely small jaw, have a tongue that they hold further back in their mouth (glossoptosis), and they have difficulties with breathing. Some of these children can be managed with sleeping on their tummies while others, with more severe forms, need to have an operation to bring their tongue forward or to lengthen their jaw to improve the airway and reduce chances for a tracheostomy.
Most children with Pierre Robin sequence are managed conservatively but for those who require surgery, it is often needed within the first week of life. These children are evaluated by our pediatric anesthesiologist, our pediatric otolaryngologist who performs a fiberoptic examination of the base the tongue and larynx, and our pediatric plastic and craniofacial surgeon who performs the osseous distraction of the mandible (Jaw lengthening procedure).
Please notice the lateral view of this child, his jaw was small enough that he could not breathe on his own immediately after birth and so an endotracheal tube was placed. We performed an osseous distraction of his mandible a few days after birth and he was able to soon breathe on his own without the aid of the tube. Here are photographs of him when he is older. Look carefully, you cannot see any scars from his surgery and notice how natural his profile is.
The cleft palate is repaired by carefully lifting the tissue of the soft palate off of the hard palate while maintaining the blood supply through the artery and vein allowing us to shift and move it to the center without tension. Tissues from the midline of the nose called the Vollmer are used to repair the nasal side of the cleft. The pallet or muscles that need to be re-oriented and repaired to allow the pallet to move up and down in a natural manner. Finally, the supper tissues of the soft palate are oriented in a way to add as much length as possible given that most children with a cleft palate have a shorter soft palate which puts them at a higher risk of hypernasality later in life if these two separate maneuvers (repairing the pallet of muscles, and lengthening the soft palate) are not performed. The real trick of the operation is to handle the tissues with extreme care, mobilize them appropriately so that they can be repaired in the midline of the pallet without tension while maintaining excellent blood flow. After surgery, your child will stay on our pediatric floor for one night before being discharged to your home the next day. We do not allow a bottle with a nipple to be used because that could irritate the palate repair so we will have your child switch to a 360 cup or similar cup without a spout to use for the three weeks after surgery. We provide a very detailed after surgery care instruction hand out for you after surgery and provide a phone number for you to call for any questions.
Postoperative complications are extremely rare utilizing our team’s protocol. One of the most problematic complications is development of a pallet of fistula where part of the palate does not repair heal so there now is a hole in the pallet communicating the mouth with the nose. Published studies show this can occur between 15 and 25% of palatoplasty however our cleft teams palate fistula reoperation rate is significantly below 1%. Our excellent results are attributed to proper patient preparation, expert completion of the surgery, and careful postoperative management management by both the pediatric floor and the family at home. Children have traveled to see us to handle complex pallet fistula problems after several attempts to repair failed at large children’s hospitals from areas including California, Oregon, Washington, Utah, Colorado, Montana and Oklahoma.
Just let your baby grow and develop. Have fun with the terrible twos, and I love them like there’s no tomorrow. We will start speech therapy at 18 months of age and schedule follow up visits with our multidisciplinary cleft lip and cleft palate team Annually or more often if necessary to carefully monitor your baby as she grows. The key areas to focus on between the ages of 14 months and three years of age is dental with proper sealants and hygiene, hearing with frequent audiology examine Examinations, and speech therapy. Speech therapy is needed to help your child adapt to their new palate. Most children do very well but there are a few who might have some mild to moderate hypernasality and can benefit from having some additional length added to their palate with a short 45 minute operation (pharyngoplasty or pharyngeal flap).
If we have done our jobs appropriately, a patient with a cleft palate should only require one plastic surgery operations between birth and 18 years of age.
We perform a palatoplasty at 13 months of age (frequently tympanostomy (eardrum) tubes are placed at the same time.
Occasionally, some patients might require a pharyngeal operation at age 3 or 4 if they have a short palate and they have persistent hypernasal speech after exhausting speech therapy options, repeat tympanostomy tube placement if they struggle with eustachian tube dysfunction and frequent ear infections, adenoidectomy if they have issues with sleep apnea, or a Le Fort I maxillary advancement with their maxilla (upper jaw) does not grow as well as expected.
